20 medical coder interview questions to hire top talent
Hiring a subpar medical coder is more than just an inconvenience – it directly threatens patient data security, regulatory compliance, and your healthcare organization's financial stability. Inaccurate medical coding leads to rejected claims, reimbursement delays, damaged reputation, and even legally binding financial repercussions.
Don’t worry – you can avoid all this. Below, we’ve compiled 20 interview questions to ask your medical coding candidates during a structured interview.
Top 16 interview questions to hire the best medical coders
The following 20 questions have been ranked in order of importance. We’ve also provided detailed sample answers – so even if you’re not a medical coding expert, you can know what to look for in candidates’ responses.
1. How would you define medical coding in your own terms, and why is ensuring its accuracy critical within the healthcare industry?
Medical coding is the process of translating medical documents into standardized codes. This means giving alphanumerical codes to diagnoses, procedures, medical services, and equipment. Accuracy in medical coding is important because a mistake could directly impact patient care, insurance claims, and medical compliance.
For example, if a patient's diagnosis of pneumonia is miscoded, they could be treated for another respiratory disease – and their insurance claim may later be rejected.
2. When learning new coding guidelines or updates to coding systems, which methods do you use to ensure you understand them and can apply them correctly in your work?
Some methods include:
Reviewing official documentation: Studying updates from CMS, AMA, and WHO for ICD, CPT, and HCPCS changes.
Attending training sessions: Participating in coding workshops and webinars offered by officially recognized organizations, such as the AAPC and AHIMA.
Practicing real-world application with peers: Implementing new guidelines in test scenarios and clarifying new rule changes with colleagues and compliance officers.
For example, when the ICD-10-CM annual updates are released, one might review the material, attend workshops to explain them, and then practice test scenarios with colleagues before going live.
3. In medical coding, how do you handle challenges related to reading legible but complex handwriting in medical records?
Here are some approaches:
Read each word carefully: Look at each word individually, examining root words, prefixes, or suffixes.
Use context clues: Cross-reference the handwriting with other parts of the patient’s records, such as lab results and imaging reports.
Standard abbreviations and terminology: Familiarize oneself with common physician shorthand and other medical abbreviations.
Ask for clarification: Reach out to the provider or medical transcription team to confirm the interpretation.
EHR tools: Use electronic health record (EHR) systems with transcription services to reduce the reliance on handwritten notes.
4. What is "medical terminology," and why is a strong understanding vital for accurately translating medical documentation into medical codes?
Medical terminology is the specialized language of healthcare with largely Latin and Greek roots. It helps to ensure precise and efficient communication about medical concepts.
A medical coder needs a strong understanding because source documents are written in medical terminology. The correct interpretation prevents ambiguity, misinterpretations, and inaccurate claim submissions.
5. Which 3 primary coding systems are used in medical coding? Explain their purposes specifically in coding patient records and claims.
The three primary systems are ICD, CPT, and HCPCS.
ICD (International Classification of Diseases):
Used for coding patient diagnoses and inpatient procedures
Helps track disease trends and healthcare statistics
ICD-10-CM is used in outpatient settings, while ICD-10-PCS is used for hospital procedures
CPT (Current Procedural Terminology):
Describes medical, surgical, and diagnostic services
Used for physician billing, outpatient procedures, and insurance reimbursement
Divided into three categories: Evaluation & Management, Surgery, and Emerging Technology
HCPCS (Healthcare Common Procedure Coding System):
Includes CPT codes but expands to cover non-physician services, medical equipment, and supplies
Used primarily in Medicare and Medicaid claims processing
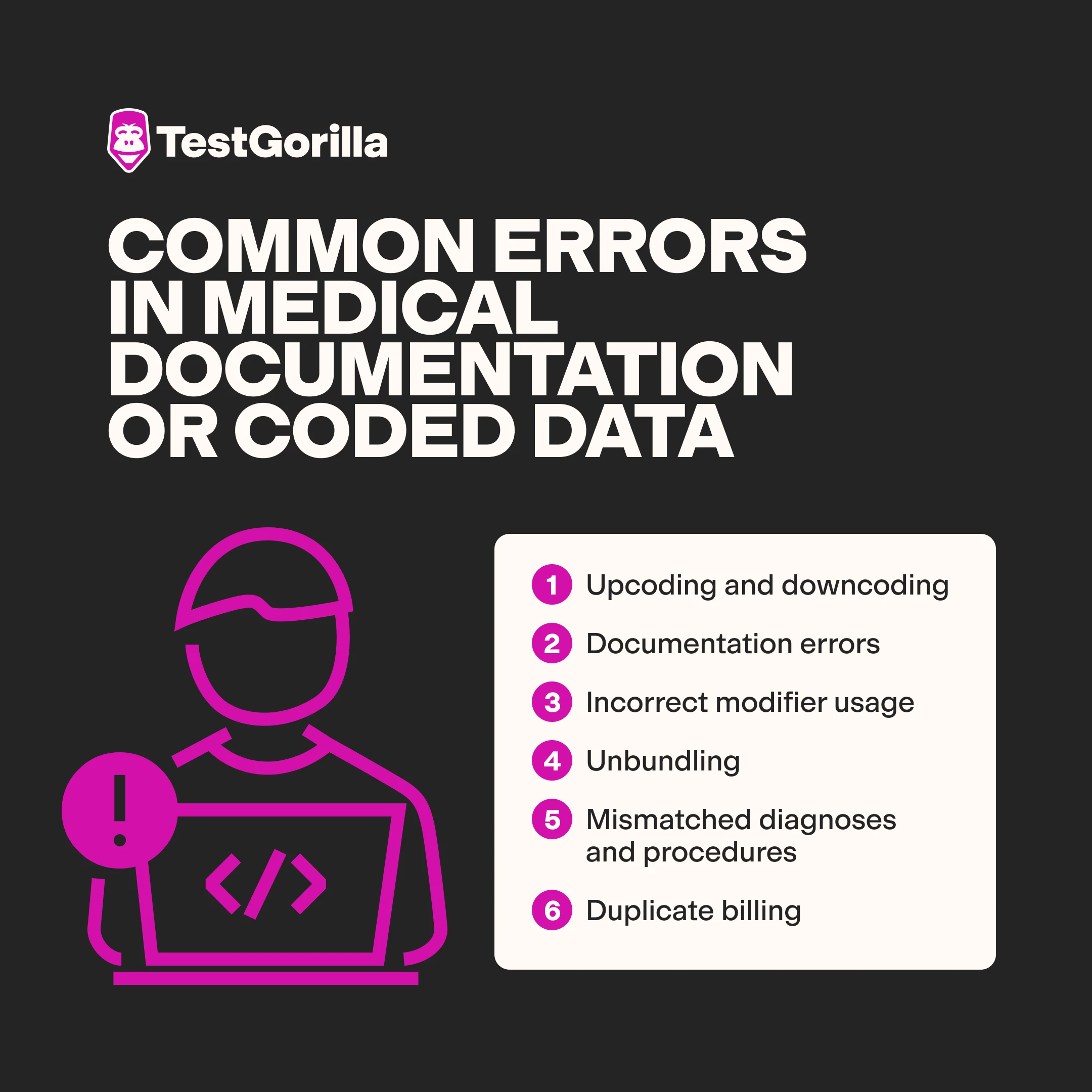
6. What are some common errors or inconsistencies in medical documentation or coded data?
Some common errors and inconsistencies include:
Upcoding and downcoding: Assigning a higher or lower level of service than documented
Documentation errors: Include missing, incomplete, vague, contradictory, or illegible documentation
Incorrect modifier usage: Assigning incorrect or missing modifiers, which could impact the payment
Unbundling: Incorrectly coding separately for services that should be bundled into a single code
Mismatched diagnoses and procedures: Using diagnosis codes that don’t match the medical necessity of the billed service
Duplicate billing: Accidentally submitting the same procedure more than once
7. What time management strategies do you use in medical coding?
Here are some strategies:
Prioritization: Handling high-risk, high-value claims first
Task batching: Grouping similar coding tasks – like E/M visits or surgical reports – together to improve efficiency
Use the latest tools: Using coding software features, EHR system efficiencies, dual monitors, and other tools to streamline workflows
Checklists: Using verification steps helps to prevent errors
8. What are the regulations governing the handling of PHI and the responsibilities of a medical coder in maintaining data privacy across different jurisdictions?
A medical coder must uphold patient data privacy and keep protected health information secure. This includes securely handling records, not unnecessarily discussing patient data, accessing information only when needed, and reporting potential data breaches.
These rules are laid out by the following jurisdictions:
HIPAA (Health Insurance Portability and Accountability Act – US)
GDPR (General Data Protection Regulation – EU)
UK Data Protection Act 2018 (aligns with GDPR but includes additional provisions for the UK)
PIPEDA (Personal Information Protection and Electronic Documents Act – Canada)
Australia’s Privacy Act 1988 and My Health Records Act 2012.
*Pro tip: Ask the interviewee specifically about your jurisdiction.
9. Explain the key distinctions between ICD-10-CM and CPT codes specifically for diagnosis and procedure billing.
The key difference is that ICD-10-CM codes report diagnoses while CPT codes describe procedures. For example, one ICD-10-CM code might be for “Type 2 Diabetes” while a CPT code might be for a “glucose test.”
Both are used for billing, but ICD-10-CM primarily justifies why the services are necessary for reimbursement, while CPT codes specify which services to bill for.
ICD-10-CM codes are primarily alphanumeric, starting with a letter. CPT codes are five digits and purely numeric.
10. Suppose you’re unsure about a code from a medical record for a diagnosis or procedure. Which resources would you use to find the correct code?
There are several resources available.
Official coding guidelines:
ICD-10-CM and ICD-10-PCS Official Guidelines for Coding and Reporting (published annually by CMS and NCHS)
CPT Assistant (AMA’s official guidance on CPT coding)
Coding books and online databases:
ICD-10-CM and CPT Manuals (latest editions)
CMS ICD-10 Lookup Tool (for US coding)
AAPC Codify or Find-A-Code for professional coders
HCPCS Level II Code Set for supplies, drugs, and durable medical equipment
Medical record review and physician queries:
Cross-reference medical records with standard coding principles
Clarify unclear documentation with the healthcare provider
Coding network and expert forums:
AAPC and AHIMA coding forums
Official AMA and CMS bulletins for updates
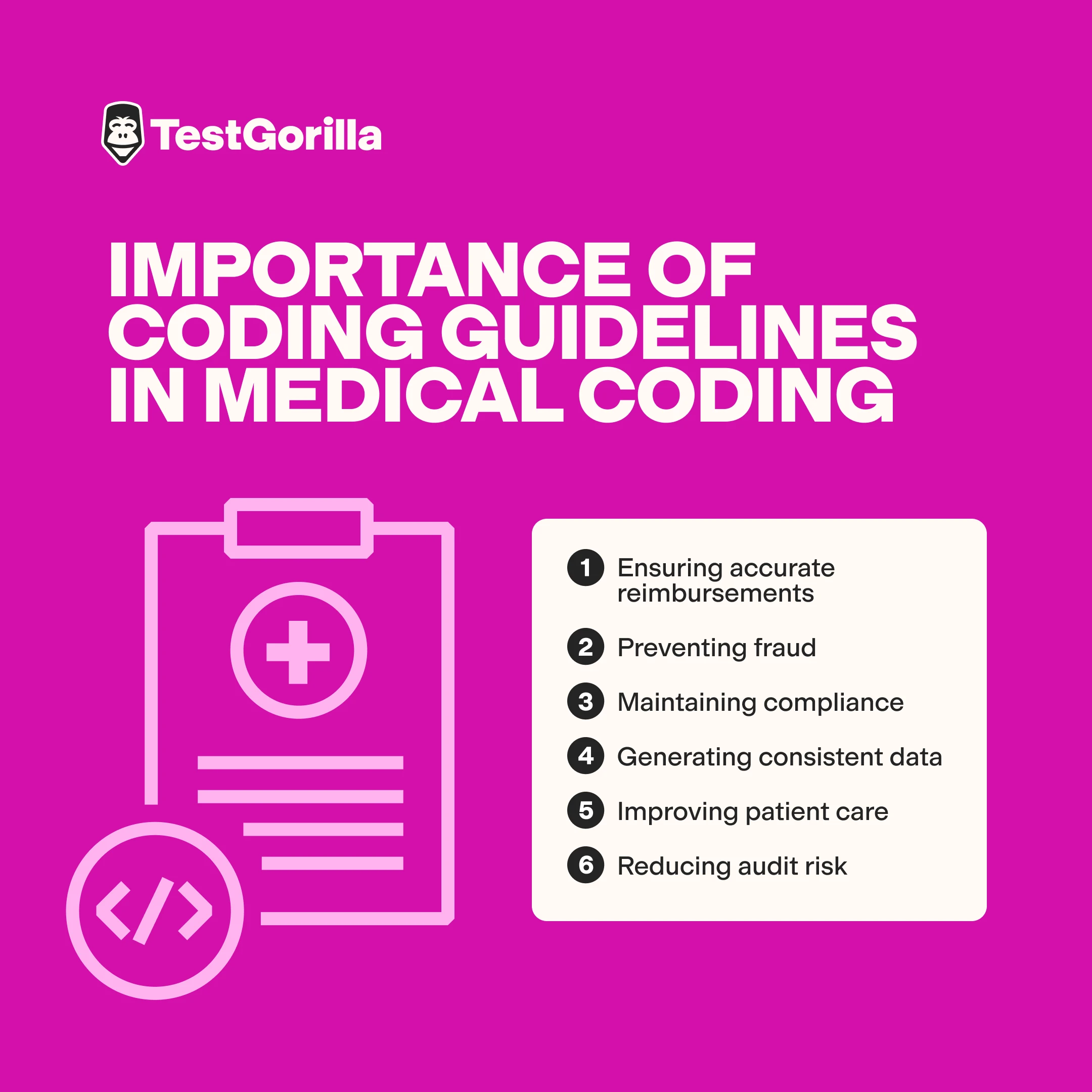
11. Describe the role of coding guidelines in medical coding and why adherence is essential for accurate coding and compliant billing.
Coding guidelines provide standardized rules for assigning codes using ICD-10-CM, CPT, and HCPCS. These have been developed by official governing bodies (CMS, AMA, WHO, and NCHS) to ensure consistency in coding practices both nationally and internationally.
These coding guidelines are crucial for:
Ensuring accurate reimbursements
Preventing fraud
Maintaining compliance
Generating consistent data
Improving patient care
Reducing audit risk
12. Name 3 key resources a medical coder should use to ensure they’re applying the most current and accurate coding guidelines.
Here are some potential key resources candidates might name:
Resource 1: Official Coding Manuals (ICD-10-CM, CPT, HCPCS Level II Codebooks)
Resource 2: Official Updates & Websites (CMS Website, AMA Website, CDC/NCHS for ICD-10-CM)
Resource 3: Coding Software/Encoders (with Integrated Guidelines)
Resource 4: Workshops run by organizations like AAPC (American Academy of Professional Coders) and AHIMA (American Health Information Management Association)
13. Explain the concept of "medical necessity" in medical coding and billing. Provide an example of a situation where demonstrating medical necessity is crucial for claim reimbursement.
Medical necessity means that the services coded are genuinely required to treat the patient's condition following generally accepted medical standards.
For example, say a doctor orders an MRI for a patient with mild lower back pain. However, the doctor doesn’t document any red-flag symptoms like neurological deficits, trauma, or cancer suspicion. The insurance provider may deny the claim, stating the MRI wasn’t medically necessary based on standard treatment guidelines.
Healthcare providers must ensure they assign the correct ICD-10-CM codes to justify the procedure and then link the diagnosis and procedure codes correctly to demonstrate the necessity.
14. Outline the typical steps a medical coder takes when coding a patient encounter, from receiving the medical documentation to submitting the coded claim.
Typical steps are:
Receive and review medical documentation, including encounter notes, progress notes, discharge summaries, operative reports, and lab/radiology results.
Abstract key information: Identify relevant diagnoses, procedures, services, and reasons for the encounter from the documentation. Highlight key terms, conditions, and procedures.
Assign codes: Translate abstracted information into appropriate ICD-10-CM, CPT, and HCPCS codes using coding guidelines and resources.
Verify and edit code: Use coding software to run code edits and checks for compliance and potential errors.
Document coding rationale: Document any coding assumptions, clarifications, or reasons for complex code choices, especially if documentation is unclear.
Submit claim (or hand off to billing): Input coded data into the billing system or pass coded encounter information to the billing department for claim generation and submission.
15. Describe the difference between "upcoding" and "downcoding" in medical coding. Explain why both are considered problematic and the potential consequences of each.
Upcoding and downcoding are coding errors that can lead to compliance violations, financial penalties, and legal consequences.
Upcoding is when a healthcare provider assigns a higher-level procedure or diagnosis code than what was documented or performed. An example is billing a complex office visit (CPT 99215) when the documentation supports only a routine visit (CPT 99213). This can lead to insurance fraud investigations, audits, fines, and legal action.
Downcoding is when a provider assigns a lower-level code than what was documented or performed, often to make it easier for a claim to be approved. An example is coding a simple wound repair instead of a complex surgical repair to reduce scrutiny. This results in lost revenue, underpayment, and financial losses for the provider.
16. What’s a coding audit in medical coding? Describe two types of coding audits that are commonly performed.
A coding audit is a review of the quality of medical coding across areas such as accuracy, compliance, and documentation. It ensures that all code types are applied correctly to reduce the risk of denied claims and legal issues.
There are two main types of coding audits.
An internal audit is conducted by the healthcare organization's coding and compliance staff. It can be prospective or retrospective.
Prospective audit: The code review is done before the claim is submitted, which allows for error correction before billing.
Retrospective audit: The code review takes place after the claim submission and payment. These audits are used to identify trends, assess overall coding accuracy, and identify past errors for process improvement.
An external review is conducted by outside entities like insurance companies, government agencies, or independent auditing firms. These reviews are always retrospective and usually focused on the payer's perspective. They’re looking for potential fraud or abuse and ensuring proper use of funds. External reviews can be more rigorous and have financial and legal consequences.
4 additional medical interview questions
Here are four more questions you might use during your interview.
Explain the importance of understanding basic human anatomy and physiology for accurate medical coding.
Identify key ethical considerations faced by medical coders.
Describe the process a medical coder should follow when they identify a potential coding error in a medical record after the claim has already been submitted. What are the key steps to ensure compliant and accurate claim correction?
Beyond entry-level coding, what specific specializations or certifications within medical coding are you interested in?
The best insights on HR and recruitment, delivered to your inbox.
Biweekly updates. No spam. Unsubscribe any time.
Find your next medical coder with TestGorilla
Need a medical coder? They should be detail-oriented, compliant, and carefully adhere to regulations.
Our medical coding interview questions will certainly help your search – but skills testing is crucial for assessing medical coding skills in practical settings. Our talent assessment platform offers various tests you can use to assess your applicants, including our Medical Coder test and Medical Billing test.
You can combine these tests with up to three other tests – including soft skills and personality tests – to create an assessment for your candidates. Then, you can use the results to shortlist top candidates for your medical coding interview.
Ready to get started? Sign up for an account.
Related posts
You've scrolled this far
Why not try TestGorilla for free, and see what happens when you put skills first.